
The most dreaded event of the delivery process is the prospect of a bleeding occurring during or after the delivery of the baby. When bleeding per vaginam follows the delivery of your baby a very prompt and detailed attention must be given to you as postpartum hemorrhage is a major cause of serious morbidity and death from specifically hypovolemia following delivery and can only be reversed by a well-thought-out care plan that must already be in place even before labor process as a standard operating procedure so that guess work and impromptu ideas and decisions are eliminated in the decision-making process as the bleeding does not give one time for frivolities before fatality ensues.
Primary postpartum hemorrhage (PPH) is defined as a loss of greater than 500ml of blood following delivery that occurs within the first 24 hours of your giving birth to your child. Primary PPH can be minor when the loss is between 500 to 1L and major when the blood loss is over 1L.
Etiology
The reason why you can develop postpartum hemorrhage can be divided into four T categories and a knowledge of these can help you to understand what you are going through and how it is important that it is addressed rightly and fast too.
1 Tone
This has to do with uterine atony which is a condition that results following delivery when the womb refuses to contract and the uterine venous sinuses remains open as a result of this leading to persistent bleeding from the placental site of detachment and the whole uterus. The womb remains floppy as a result of this inability to contract and continues to bleed.
2 Trauma
Labor and delivery is associated with trauma and traumatic injuries from the birth process both from the baby and the instruments used to expedite the labor process. All these injuries on the birth canal are associated with bleeding as the baby is delivered and range from cervical injuries to vaginal injuries to episiotomies and perineal injuries. If the amount of bleeding from these birth canal injuries is not adequately addressed and prevented it can lead to a blood loss that can be symptomatic and result in PPH.
3 Tissues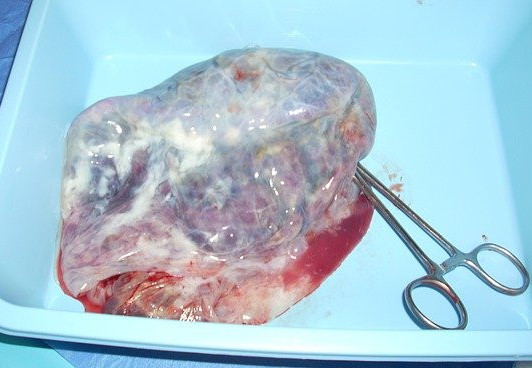
When you deliver the baby, the next thing that gets to be delivered is the placental tissue and membranes. When the placenta is incompletely separated or remnants of the placental tissues or membranes are not delivered completely it leads to inability of the uterus to contract well leading to a bleeding episode and postpartum hemorrhage.
4 Thrombi
When we talk about thrombi, we are referring to your body’s blood clotting mechanism which can be deranged in pregnancy as a result of many factors leading to the inability of the blood to clot. If this persists through labor and delivery of your child, it can lead to development of PPH as a result of the development of coagulopathies following delivery.
Risk factors
The risk factors to the development of Primary PPH traverse the causes listed above and by knowing your risk factors it will help you to plan to prevent the likelihood of your development of postpartum hemorrhage
Risk factors to uterine atony are as follows
Maternal age above 40, BMI greater than 35, Asian and African ethnicity, Primiparity and grand multiparty, Anemia in pregnancy, Uterine over distension like multiple pregnancy, Polyhydramnios and big babies, Prolonged labor and induction of labor.
The trauma risk factors include
Instrumental deliveries like vacuum extraction and forceps deliveries, episiotomies and perineal tears and vaginal lacerations and cervical traumas
The risk factors related to tissues
Here you have to deal with issues related to retained placental tissue following delivery, incompletely separated placenta, poor management of 3rd stage and secondary placenta
The risk factors for thrombi
The considerations include conditions like placental praevia, placental abruption, hypertension and preeclampsia and acquired coagulopathies like DIC and HELLP syndrome.
Pathophysiology
During your pregnancy there is a marked increase in the plasma volume which rises from 4 to 6 liters, an increase of almost 50%. This rise in blood volume is not compensated with a commensurate rise in the red blood cells leading to what we call dilutional anemia in pregnancy in the event that you do not make concerted effort to improve your nutritional status to make up for the shortfall in red cell production by the body.
This increase in plasma volume is necessary to maintain perfusion of the uterus and placental bed which receives about 15% of the cardiac output.
In labor, as the blood traverses the unique blood vessels of the uterine muscles with its latticed network, this enhances contraction of the muscles with subsequent occlusion of the vessels passing through these muscles in a living ligature style.
This contractile action on the vessels prevents postpartum bleeding and hemorrhage as the blood vessels are kinked and compressed with each muscle contraction culminating in complete occlusion with the delivery of the placenta and sustained uterine contraction post delivery prevents primary postpartum hemorrhage.
Any disruption to this normal physiology like in uterine atony will lead to PPH. Genital tract trauma during delivery will lead to bleeding as a result of the increased blood flow to the perineum in pregnancy and labor and delivery process.
Prevention
The prevention of postpartum hemorrhage will be addressed by tackling the risk factors that are associated with this condition but it must be known also that about 20% of all cases of PPH are not related to any identifiable risk factors hence there needs to a clear cut care plan for the management of PPH that is readily implementable at all times.
The most important aspect to the prevention of PPH is the active management of the third stage of labor (AMTSL).
AMTSL involves the following:
- Use of oxytocics example pitocin immediately after the delivery of the anterior shoulder of your baby
- Controlled cord traction to deliver the placenta
- Uterine massage after the delivery of the placenta
The general preventive measures that should be instituted in the care of patients
Antenatal:
Screen and treat anemia
Screen and review patient genotype to rule out sickle cell disease
Rule out and determine religious affiliations like Jehovah witnesses that do not accept blood and its products
Intrapartum
Aside active management of your 3rd stage of labor,
Avoid routine episiotomies
Avoid routine instrumental deliveries
Avoid prolonged labors
Track and manage postpartum blood losses to determine when it is becoming critical.
Postpartum
Nipple stimulation and breastfeeding has been known to cause release of oxytocin naturally into the bloodstream from the posterior pituitary hence when the mother is encouraged to put the baby to the breast immediately postpartum it will help to release oxtytocin helping to contract the uterus and acting as a preventive mechanism against PPH in the immediate postpartum period.
Uterine massage also has the effect of stimulating the uterus to contract and keep the vessels within the muscles of the uterus compressed and constricted preventing atony and bleeding.
Care plan
The care of primary postpartum hemorrhage will depend on the identified factor that is responsible for the bleeding in the first place whether it is due to trauma, tone, tissue or thrombus. Your doctor should always be on hand to determine the cause, classify the extent of the bleeding and determine the appropriate measure to institute ranging from medical therapies, surgical interventions, and the use of medical devices at different levels of the treatment of PPH like the non-pneumatic anti-shock garment for managing PPH outside the hospital setting before referral to the uterine baloon tamponade to the Sengstaken-Blakmore tube.
Conclusion
It must be noted that postpartum hemorrhage is an emergency unplanned event in the labor and delivery process and for there to be a successful outcome in cases of obstetric hemorrhage, it should always be anticipated in every labor as a possible complication and hence it must be pre-planned for and the care plan carefully stated and spelled out in the form of a protocol of management so that it can help save lives and reduce the mortality and morbidity associated with this event.
Dr Mawa
To your postnatal health and freedom
mypostnatalmanagement.com
Please if you have any questions, comments, ideas, suggestions or experiences you want to share about primary postpartum hemorrhage kindly use the comments box below.




This is very helpful information about primary postpartum hemorrhage. This information is very important in making sure that the new mother gets the healthcare she needs in a timely manner. There is no time to waste when dealing with any kind of hemorrhage, and it’s helpful to know what could happen. The best help is always prevention, so thank you for giving actionable items that can proactively prevent problems!
Thank you. Primary PPH is a fast killer and preventive strategies are always better when well anticipated as it will lead to reduced morbidity and mortality from this condition
This is very helpful information about primary postpartum hemorrhage. This information is very important in making sure that the new mother gets the healthcare she needs in a timely manner. There is no time to waste when dealing with any kind of hemorrhage, and it’s helpful to know what could happen. The best help is always prevention, so thank you for giving actionable items that can proactively prevent problems!
Postpartum hemorrhage is a very familiar term because it happened to me after delivering my firstborn via cesarean. I was already wheeled into the recovery room after a successful operation and was given a pain reliever. But when the nurse came to assess the pain, she asked me to scale it from 1-10. It’s supposed to be lower, but I scaled it to 8. It was very painful even if I already had the pain reliever. The doctor came, pushed my stomach and a gush of coagulated blood came out. The doctor explained that I was hemorrhaging after the delivery because the placenta was very attached to the uterine wall and they were not able to remove all the coagulated blood inside! What a scary experience, thank God all went well.
Waoh . Thank God it ended well and the prompt attention by the doctor. It is not common to have postpartum hemorrhage following cesarean section as it could affect the stitches worsening the problem. I guess the placental attachment explanation is reasonable as placental adhesion either accreta or the others can lead to atony and poor contraction. thank you for sharing this experience
Postpartum hemorrhage is a very familiar term because it happened to me after delivering my firstborn via cesarean. I was already wheeled into the recovery room after a successful operation and was given a pain reliever. But when the nurse came to assess the pain, she asked me to scale it from 1-10. It’s supposed to be lower, but I scaled it to 8. It was very painful even if I already had the pain reliever. The doctor came, pushed my stomach and a gush of coagulated blood came out. The doctor explained that I was hemorrhaging after the delivery because the placenta was very attached to the uterine wall and they were not able to remove all the coagulated blood inside! What a scary experience, thank God all went well.
Very scary situation when you have to deal with PPH especially primary as it presents as a continuation of the crisis associated with delivery in an upper scale and thank God the doctor was proactive as that is usually a thin line between a successful outcome and disaster.